As parents, educators, and health professionals grapple with the rising rates of adolescent obesity, new research shines a spotlight on an often-overlooked factor: sleep. A systematic review by researchers at the University of St. Andrews explores the complex relationship between various sleep dimensions and obesity in adolescents. The findings, published in Sleep Medicine Reviews, offer insights into how bedtime habits and sleep quality may influence body weight and health.
Sleep and Adolescent Obesity: A Growing Concern
Obesity among children and adolescents has skyrocketed from 4% in 1975 to 18% in 2016, according to global studies. While diet and exercise are well-known contributors to weight gain, sleep patterns are emerging as a significant factor. Poor sleep can lead to a cascade of effects, including reduced energy levels, unhealthy eating habits, and hormonal imbalances that increase appetite.
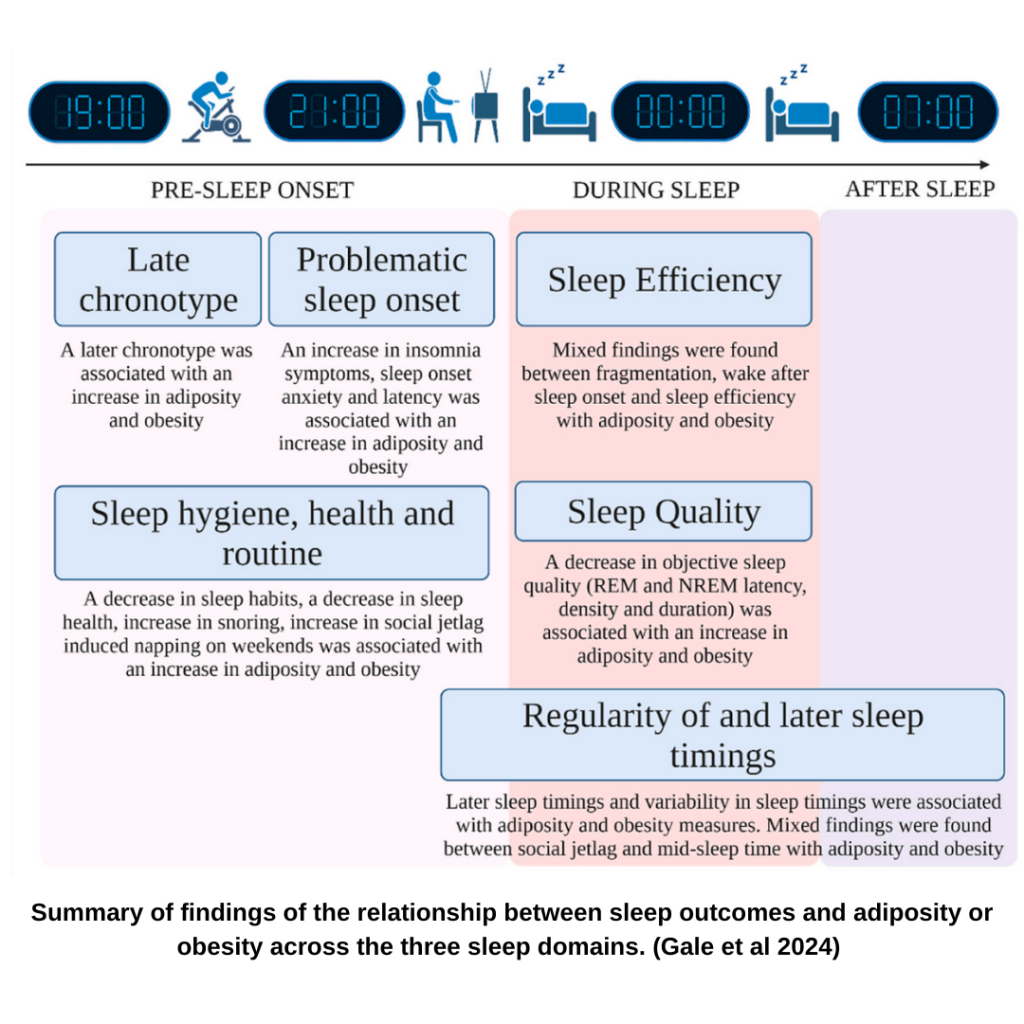
The review examined 89 studies from 27 countries, focusing on adolescents aged 8 to 18. It identified three key “sleep domains” that affect weight:
- Pre-sleep behaviors: Bedtime routines, sleep hygiene, and variability in sleep timing.
- During-sleep factors: Sleep quality, efficiency, and disturbances.
- Post-sleep outcomes: Wake times, social jetlag, and daytime sleepiness
Key Findings: How Sleep Influences Weight
- Late Bedtimes and Chronotypes
Adolescents with “evening chronotypes” (those who prefer staying up late) were more likely to be overweight or obese. Late bedtimes shorten sleep duration and disrupt the body’s natural circadian rhythms. This misalignment affects hormones like leptin and ghrelin, which regulate hunger and satiety. - Irregular Sleep Schedules
Variability in sleep timing—such as sleeping late on weekends—was linked to increased body fat and waist circumference. This “social jetlag” creates a mismatch between the body’s internal clock and external routines, leading to poor dietary choices and decreased physical activity. - Sleep Quality Matters
Poor sleep quality, marked by frequent awakenings or difficulty staying asleep, was associated with higher body mass index (BMI) and increased fat mass. Sleep disturbances also disrupt REM sleep, crucial for memory and emotional regulation, potentially increasing stress-related eating.
Practical Tips for Better Sleep
The good news is that most of these factors are modifiable. Here are some practical tips for parents and teens to improve sleep and potentially reduce obesity risk:
- Establish a Consistent Bedtime Routine: Encourage regular sleep and wake times, even on weekends.
- Limit Screen Time: Reduce exposure to screens at least one hour before bedtime to prevent blue light from interfering with sleep hormones.
- Promote Sleep Hygiene: Create a calm, comfortable sleep environment free from distractions.
- Encourage Healthy Eating Habits: Avoid caffeine and heavy meals before bedtime, as they can interfere with sleep quality.
Why This Research Matters
This study underscores the need to consider sleep in adolescent health interventions. While traditional approaches focus on diet and exercise, addressing sleep habits could amplify the effectiveness of obesity prevention programs.
A Call to Action
Parents, educators, and policymakers must take sleep seriously when addressing adolescent obesity. Schools can start by reconsidering early start times, which often clash with teenagers’ natural sleep cycles. Public health campaigns should include sleep education alongside nutrition and physical activity guidelines.
As we navigate the challenges of modern living, understanding the intricate relationship between sleep and health is more critical than ever. By prioritizing good sleep habits, we can help the next generation achieve healthier, more balanced lives.




